By Blanca Martínez and Andrés Gerlotti
Currently, those suffering from bone or cartilage damage can opt for metal implants for treatment, prostheses that last approximately fifteen years. But now that patients are living longer, they need implants that can function for the rest of their lives.
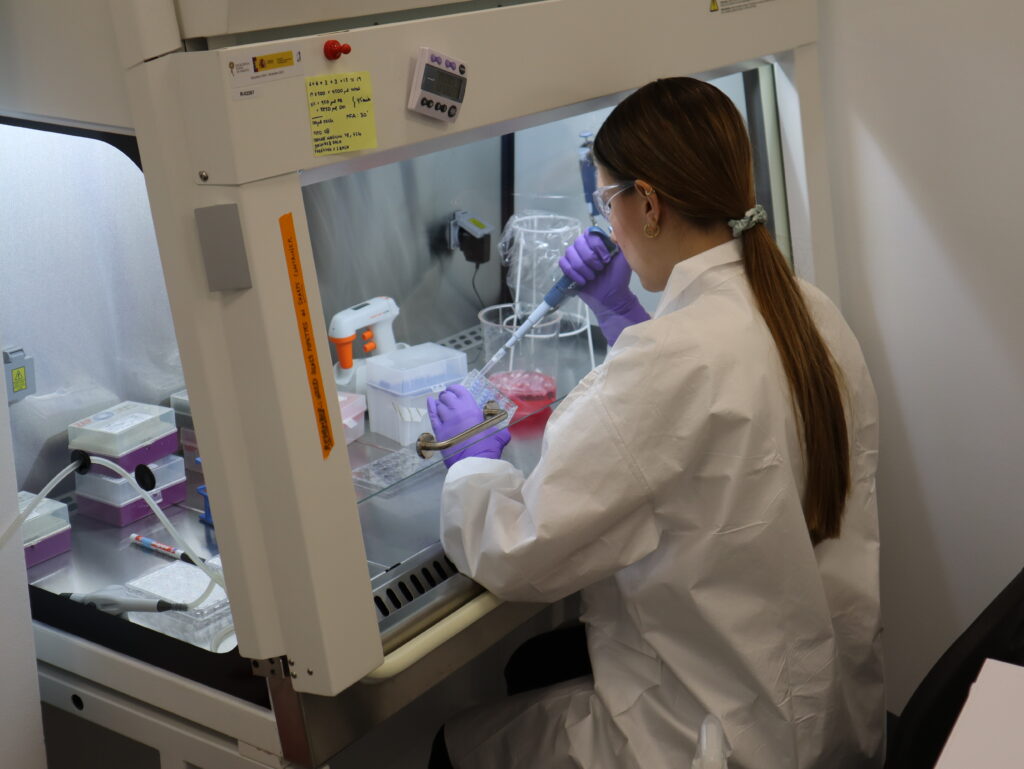
At IMDEA Materials Institute, one of the seven IMDEA Centers of Excellence promoted by the Community of Madrid, new materials are being researched and developed to regenerate damaged tissues and restore their function.
Dr. Jennifer Patterson, a native of Philadelphia, USA, is the scientist leading the Biomaterials and Regenerative Medicine research group at the Institute. Her work is divided into two areas. The first deals with the development of new materials for medical applications. The second focuses on regenerative medicine, developing materials that help tissue regeneration.

Within these two areas, the research group is focused on applications for bone tissue and, as a result of COVID-19, also for lung tissue. They work with two types of materials, biological derivatives extracted from animal or human donor tissues, and synthetics. Each has advantages and disadvantages: the biologically derived ones have intrinsic biological activity that helps cell function, but they can also represent disadvantages because of the possibility of causing diseases or compatibility problems between the animal tissue and that of the human patient.
“That makes it difficult to produce these types of materials,” Dr. Patterson says. “I’m interested in developing synthetic materials that mimic the properties of the biological ones, so that we can have the bioactivity and function, but with the ability to create it entirely in the lab and achieve greater control.”
“We are still far from being able to replace an organ. There are tissues in which cells grow quite well, such as in bone. For example, if someone breaks one, in most cases, they just have to put it back together so that the ends are in contact, and the bone grows and heals on its own. However, it is more difficult when it comes to operations such as heart surgery, because the muscle cells found in the heart have no regenerative capacity.”
Related to regenerative medicine, another objective at IMDEA Materials Institute is to prevent a recipient’s immune system from attacking the implant. According to Dr. Patterson, when tissue or cells from one person are transplanted into another, there will be reactions in the body that will try to annihilate these foreign cells. That is why, when a patient receives a transplant, he or she must have a certain compatibility.
“But even with a match,” Patterson explains, “you will have to receive immunosuppressive drugs to prevent that immune system response. Instead of combining cells, we work to use the patient’s own cells, and thus prevent the aggressive immune reaction.”
Potential applications
Patterson and her team’s research is still a long way from being commercialized. She explains that they have only been doing research at IMDEA for two years and that, “normally, the research process leading to a commercial product takes a long time. The simplest ones can take less than five years, but the more complicated ones can take up to fifteen years and have many necessary steps such as animal and human testing and approval by the authorities”.
The study that is closest to proof-of-concept involves the development of implants that change their shape once inserted into the body.
“It is a very ambitious project and our goal is that in four years we will have been able to test it in animals,” says Patterson. In addition, the doctor emphasizes that, for the moment, her team is focused only on the early stages of research and is not interested in testing in humans.
The ultimate goal of medical regeneration is to end up creating entire organs, even with the patient’s own cells to avoid rejection of the implants, but it is “difficult to know how long it will take for this to happen,” she adds. “Slow and steady, but someday it will come,” clarifies Javier García Pérez, a researcher on Patterson’s team.
A science that does not harm animals
The ‘Organ-on-chips’ with which work has recently begun at IMDEA Materials Institute are models of human organs on a reduced scale. “What we want to do is to subject simulated tissues, grown by us on microfluidic chips, to all kinds of tests on a microscopic scale,” explains Patricia Paramio, a researcher on Patterson’s team.
This type of technology allows them to simulate human tissues and test drugs at a “real and reliable” level. The idea for the future is that, “if another disease like COVID-19 comes along, we will be able to test the effect of a drug on diseased cells in real time,” says Paramio. And, in addition to obtaining results quickly, “you do it in a device without harming any animal,” adds the researcher.
Two of the Institute’s most important projects in relation to the regenerative medicine field are BIOMET4D, a European Innovation Council Pathfinder funded project under the umbrella of the Horizon Europe programme (grant agreement No 101047008) and MAMAP-CM, a project funded by the Community of Madrid and by the Regional Development Fund of the European Union “A way of doing Europe”.
The latter financed as part of the Union’s response to the COVID-19 pandemic, through the agreement signed between the Community of Madrid and the IMDEA Materials Foundation to finance research activities on SARS-COV 2 and the COVID-19 disease financed with the REACT-EU resources of the European Regional Development Fund.